About School Based Mental Health
Comprehensive school mental health programs work to address the mental wellbeing needs of students via culturally-responsive services throughout a continuum of levels:
*Individualized services = access to clinical therapy & consultation for students with more complex challenges.

This continuum of services helps students navigate life’s challenges with resiliency using various strategies:
- Conflict resolution
- Self-regulation
- Communication of needs and boundaries
- Mindfulness
- Mental health literacy
Programs and services are implemented by school staff, including school counselors, social workers, psychologists, administrators, nurses, and special educators.
Supports may also include licensed mental health therapists available on-site or via telehealth during the school day.
Classroom teachers and parents are key collaborators.
Comprehensive school mental health supports the mission of schools: learning! Young people who receive appropriate mental health supports have improved academic achievement & are more likely to graduate.

Nearly half of Wisconsin high
school students report anxiety.
More than one-fourth feel depressed.
In the wake of the COVID-19 pandemic, Wisconsin students report increased levels of stress, anxiety, and depression. Many expressed a need for more mental health resources at their school, specifically counselors, therapists, and psychologists.
If I had free access to mental health resources through my school,
WI student
I would take advantage of it.
In an analysis comparing pediatric healthcare claims from 2019-20, two Wisconsin findings stand out:
- Intentional self-harm claims for the 13-18 age group increased more than 100% from March 2019-2020.
- Wisconsin ranked among the top 5 states in the nation for the most intentional self-harm claims ages 6-22.
Experiences of mental health challenges and the likelihood of receiving treatment differ among children in diverse populations. For example, 11% of Black children needed but did not receive treatment in 2018, as compared to 2% of white children.
School-based mental health services increase accessibility, reduce barriers, and improve equity of access to promote well-being and achievement
Public school students spend most of their time at school. Because of this, teachers & school counselors are often the first to identify or hear about mental health challenges.
For many families, it is easier to have students access care at school than it is at home or after school. Transportation, student extracurricular involvement, and caretaker availability can all be barriers to accessing care outside of schools.
Connecting mental health services to academic goals can help destigmatize therapy and create a special incentive for families to engage.
Outcomes are measured in many areas, including academic performance, standardized testing results, attendance, behavioral referrals and suspension, and psychosocial data.
A 2017 study demonstrated that Wisconsin students receiving school-based mental health services were significantly more likely to show growth on the START Math test than students in the study’s control group. Additional findings included increased attendance, decreased days of suspension, and improved results on the Strengths and Difficulties Questionnaire.
WORKFORCE
Widespread workforce shortages throughout Wisconsin impact both student services staff and licensed mental health clinicians. In fact, Wisconsin falls short of nationally recommended ratios for school psychologists, counselors, and social workers. Increased funding is needed to improve the student to pupil services staff ratio.
INSURANCE
Despite districts’ desires to provide universal access to care, students with private insurance plans may encounter barriers to accessing service, such as:
- High deductible health plans that make it difficult for families to afford behavioral health services. Since 2013, the percent of WI private-sector employees with high deductible insurance plans has increased from 35% to 57%, exceeding the national average.
- Restricted insurance networks that do not include the school-selected providers and/or have limits on the location for mental health service delivery, such as teletherapy.
- In order to increase access to one-on-one therapy services, many schools contract with Qualified Treatment Trainees (QTTs): experienced clinicians still completing certification hour requirements. While MA covers these QTT services, private insurance providers do not.
NAVIGATION
Even when students’ mental health needs are identified via referrals and screenings, families may face additional barriers to accessing care:
- stigma of treatment
- lack of understanding
- unclear options
- paperwork (time)
- incompatible insurance
- deductibles, co-pays
- difficulty scheduling
When funding is available, districts can employ a School Mental Health Navigator who supports families along their journey to treatment.
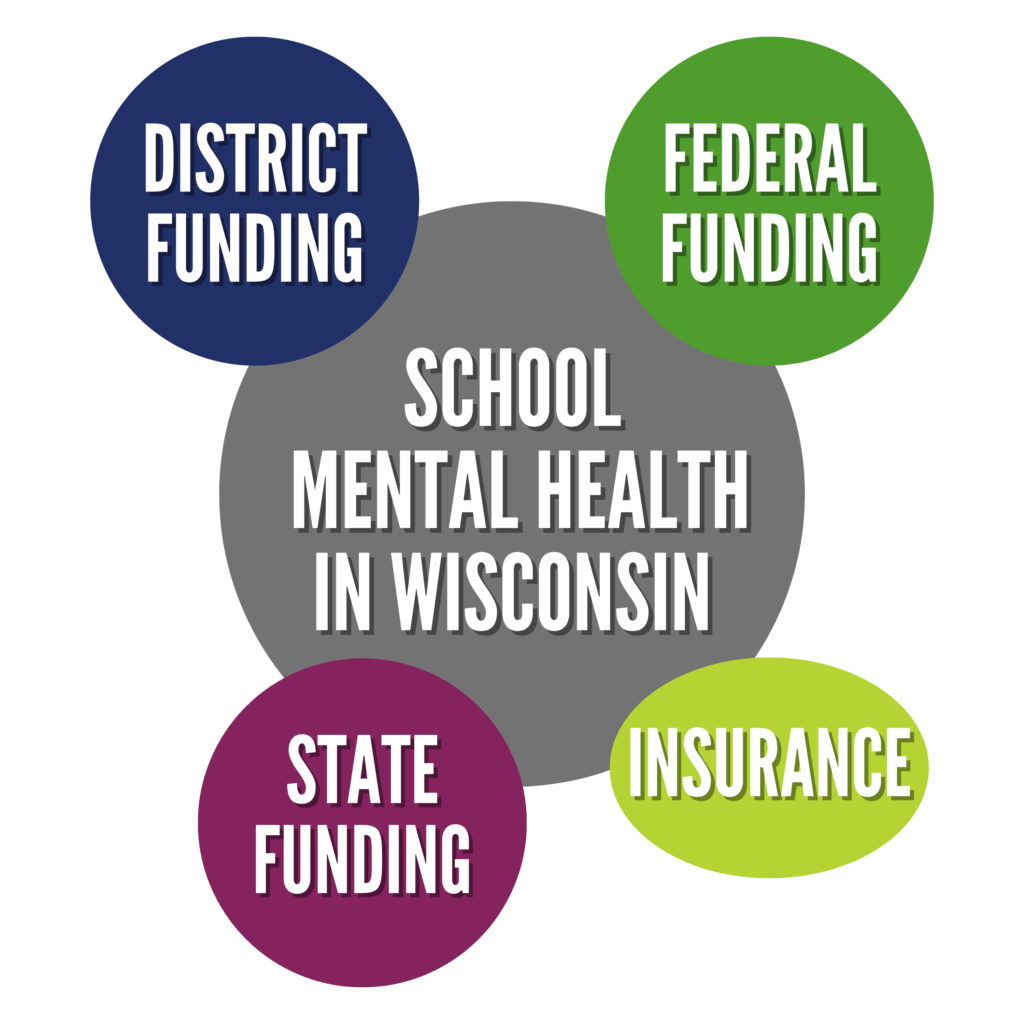
How is School Mental Health funded?
- School districts and foundations provide significant funding support for school-based mental health initiatives.
- In recent years, districts across the state have also received targeted federal & state grant funding to support services.
- Access to individual and group therapy services relies heavily on students’ health insurance coverage.
DISTRICT FUNDING
In order to initiate & sustain school mental health collaborations, many districts commit their own levy dollars to support school staff, training, assessments and contracts with therapy providers.
- Schools leverage local funding including Community Services Funds (Fund 80) to the degree that such resources are permissible.
- In addition, local foundation dollars committed through United Way and other philanthropic partners (including the Wisconsin Partnership Program and the Advancing a Healthier Wisconsin Endowment) have enabled local collaborations to scale up and consider long-term sustainability.
- Some districts have formed targeted foundations to channel donations for ongoing programming.
STATE FUNDING
The WISH Center (Wisconsin Safe and Healthy Schools) delivers state-wide training for alcohol, tobacco, drug, violence, and bullying prevention. It provides professional learning opportunities and technical assistance, supporting schools as they plan, implement, and
evaluate program efficacy.
The School-based Mental Health Grant Program is a competitive statewide grant program. In 2020, 106 grantee districts each received up to $75,000 in funds to collaborate with community mental health agencies to support students’ mental health.
Via this grant, 52,470 Wisconsin students received support from a school mental health provider (School Social Worker, Psychologist, Counselor or Nurse). ***
This grant allowed 13,630 referred students to access at least one appt. with a community mental health provider. ****
FEDERAL FUNDING
Project AWARE (Advancing Wellness and Resiliency in Education) is a competitive five- year grant from the federal Substance Abuse and Mental Health Administration (SAMHSA). The grant targets efforts within three selected Wisconsin school districts to strengthen mental health awareness and to replicate effective strategies statewide.
ESSER Fund (Elementary & Secondary Emergency Relief), part of the Coronavirus Aid, Relief, and Economic Security (CARES) Act, provides services & supports to public & private schools to build capacity of school staff to provide mental health services & respond to changes in needs due to COVID.
The School-Based Mental Health Professionals Grant Program provides grants to increase the number of qualified mental health service professionals that provide school-based mental health services to students in local educational agencies with demonstrated need.
INSURANCE
Third party billing to insurance is a critical funding source.
Covering 1 in 3 children in WI, Medicaid (MA) is an important payer supporting individual and group therapy services for children referred for a Tier 3 service.
In recent years, Medicaid has improved reimbursement rates and availability of services for eligible students, including a billing code that supports provider time to consult with school staff, teachers, and parents regarding a student’s mental health treatment plan.
*This is aggregate data from the 2019-2020 End of Year Reports submitted by grantees. The state statute authorizing this grant competition does not include any data collection or reporting -requirements. Grantee plans are locally determined, and the Department of Public Instruction does not monitor grantee outcomes.
**Grantees were given a list of items to select from. This list is not exhaustive, as grantees are doing other activities not listed on the report.
***Note that this number counts students only once, even if seen multiple timesby multiple professionals. Mental health contact was defined at the local (not state) level. These numbers do not reflect a specific environment. For some grantees, only the high school or elementary school are represented, and for others, these numbers may reflect the whole district.
****This number reflects the number of students referred who make it to at least 1 appointment. This number may not be accurate due to confusion about collection. Some grantees have limited access to treatment providers. This does not collect information about why students do not access treatment (transportation, insurance, family follow-through, lack of providers, etc.)
Community providers and school providers (school counselors, nurses, social workers and psychologists) work together in meaningful ways to promote positive mental health outcomes for students.
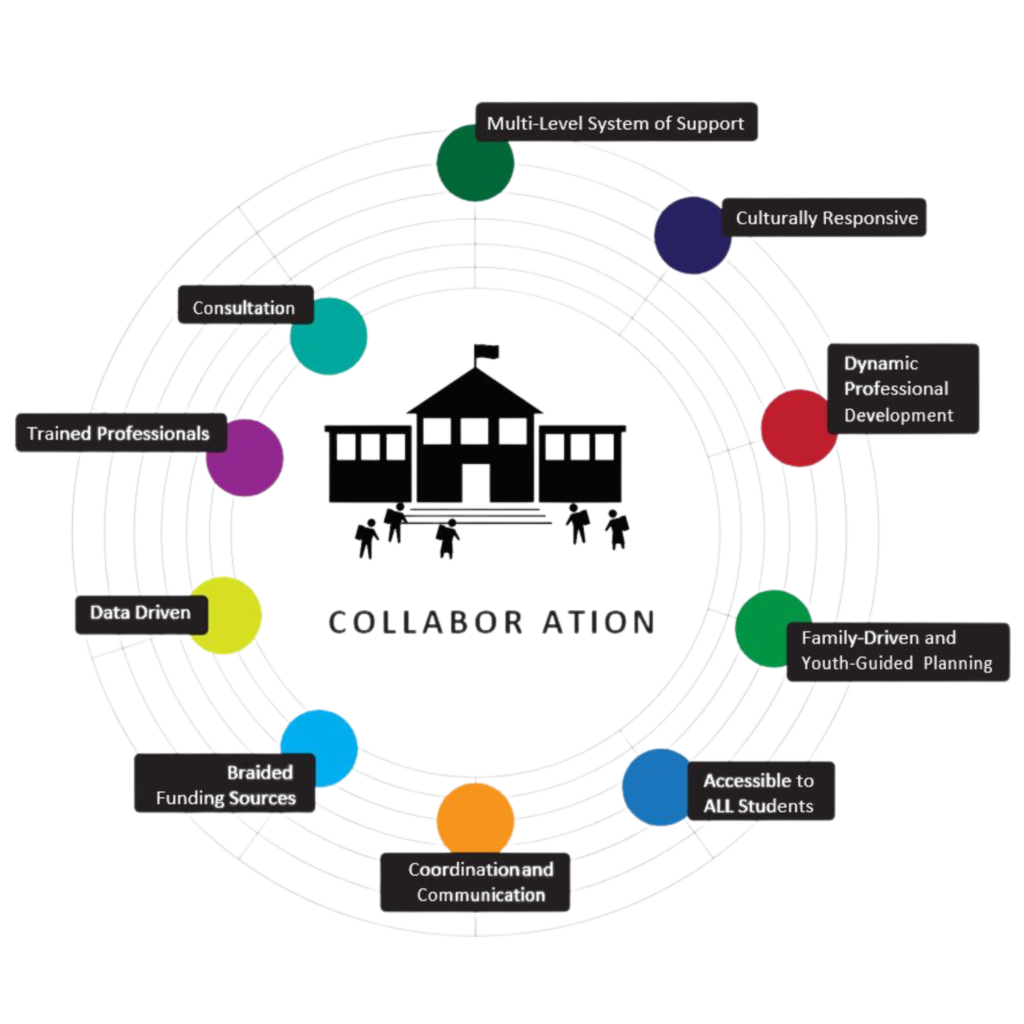
Multi-level system of support
The processes for referral, assessment and counseling are established and integrated within the school problem-solving process. Interventions are designed based on student needs. Treatment focuses on reducing barriers to development and learning, is family- and student-oriented, developmentally appropriate, culturally responsive and respectful,
strengths-oriented, and based upon evidence of positive impact.
Cultural Responsiveness
Cultural responsiveness is “the ability to honor and respect the beliefs, languages, interpersonal styles, and behaviors of individuals and families receiving services, as well as staff members who are providing such services. Cultural responsiveness is a dynamic, ongoing developmental process that requires a long-term commitment and is achieved over time.” (SAMHSA)
Dynamic Professional Development
Professional development efforts are aligned and integrated as unified initiatives, including: PBIS, mental health, alcohol or other drugs, suicide prevention, trauma sensitive practices, resiliency, and social-emotional learning. Everyone who works with students and families is invited to professional development opportunities.
Family-Driven and Youth-Guided Planning
Fully partnering with families and students is central to ESMH success. Empowerment starts with school leadership setting a standard, in both words and actions, of treating all students and families with positive regard. Support plans are family-driven, in recognition
of parent expertise about their child, and youth-guided in recognition of the information
youth can offer about themselves, once asked and included.
Accessible to ALL students
Services are accessible to all students regardless of payer source (insurance source), ability to pay, or protected status.
Coordination and Communication
When integrating community providers into the schools, a process is developed to address communication, role definition, and the sharing of responsibilities. Community providers understand the culture and expectations within the school environment, and school staff understand rules and regulations that govern clinicians. Ongoing meetings between the school and the agency are scheduled to address inevitable challenges and deepen collaboration. All partners must establish a continuous communication loop of information sharing with the appropriate releases of information.
Braided Funding Sources
Multiple revenue streams should be accessed, including insurance or Medicaid. The most
stable plans rely on maximizing third party billing and using other sources of funding (state, county or city government, grants, United Way support and agreements with HMOs) to cover non-billable, ancillary services such as professional development, consultation, and providing care for uninsured students.
Data Driven
School staff and clinicians have a data collection plan which may include measuring academic achievement, suspensions, expulsions, and health outcomes, as well as reported changes in attitudes and beliefs toward those living with mental health issues. Student and family satisfaction surveys as well as teacher/school process evaluations help inform schools and providers of perceived program strengths and weaknesses. Data collection and continuous quality improvement contribute to the success of the program, and provide information that is invaluable in securing braided funding.
Trained professionals
In collaboration with pupil services staff who are trained school mental health professionals, community providers are licensed mental health professionals or appropriately supervised qualified treatment trainees in good standing under the Department of Safety and Professional Services. All mental health professionals will be knowledgeable and follow the ethical standards of their professions including: clinical supervision, adherence to confidentiality, and a grievance procedure.
Consultation
Consultation is central to the ESMH model, either in person or by phone, with parents/
caregivers/foster families, youth-serving professionals (child welfare, juvenile justice,
crisis counselors, school staff, care coordinators), and health care providers (psychiatrists,
primary care doctors, nurse practitioners, hospital discharge planners and social workers). In-person consultation about how to best meet student’s social-emotional needs occurs regularly with individual educators, educator teams, wraparound teams, and at hospital discharge and IEP meetings. Best models of consultation focus on care coordination with shared strategies between home, school and youth-serving professionals.